Peroneal Tendonitis
(AKA: Peroneal Tendon Tear, Attritional Peroneal Tendon Tear)
Summary
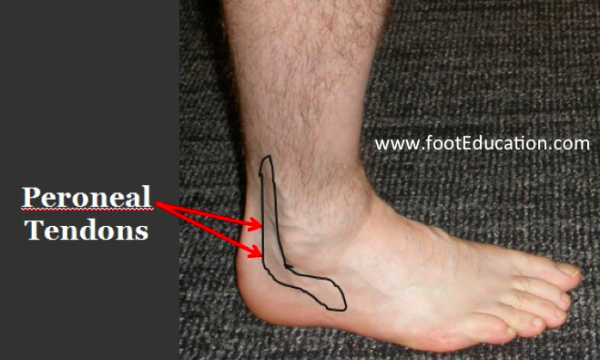
Peroneal tendonitis is an irritation to the tendons that run in a groove behind the bony prominence on the outer aspect of the ankle. Symptoms of peroneal tendonitis include pain and swelling in the outside back part of the ankle (Figure 1A) that may be worsened with activities. The two tendons involved are the peroneus longus and peroneus brevis. The tendonitis usually occurs because over time these tendons are subject to excessive repetitive forces during standing and walking. Certain types of feet (ex. high arched feet or feet with misaligned heels that are inclined or tilted inwards) tend to increase the repetitive forces that the peroneal tendons are exposed to, and predisposed these individuals to the risk of peroneal tendonitis. Treatment of peroneal tendonitis is aimed at decreasing symptoms and correcting any precipitating factor. Non-operative treatment may include: anti-inflammatory medications, activity modification, ice, muscle strengthening, ankle bracing, and/or specific types of shoe inserts or orthotics. Occasionally surgery is beneficial.
Peroneal Tendonitis Summary Handout
Clinical Presentation: Peroneal Tendonitis
Patients with peroneal tendonitis present with pain and occasionally swelling in the outside and back (posterolateral) part of the ankle (Figure 1A and 1B). This tends to be a chronic condition, gradually becoming more painful over time. However, sometimes patients will report an activity that aggravated their symptoms relatively quickly.
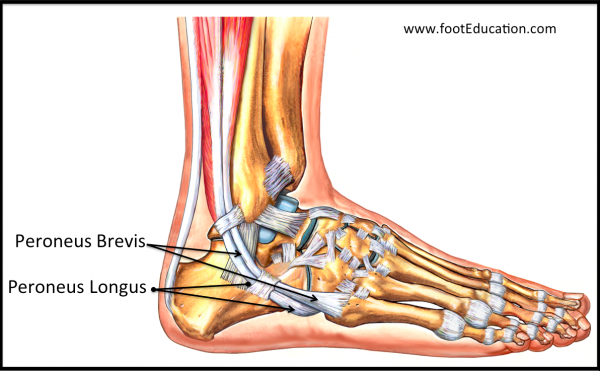
The peroneal tendons run behind the prominent bone on the outside of the ankle. There are two tendons, the peroneus brevis and the peroneus longus. These tendons help to control the position of the foot during walking. They are also responsible for the muscle contraction that moves the foot out to the side (eversion of the foot). Peroneal tendonitis is an irritation to these tendons. Essentially, the tendons are repetitively overloaded creating wear and tear on the tendon with the subsequent inflammatory response (attempt at healing) creating pain and discomfort. This inflammatory response is the reason why patients with peroneal tendonitis often have startup pain –pain first thing in the morning. The mechanism by which this condition develops is akin to a rope that is repetitively overloaded.
Just as a rope can become frayed- some patients with peroneal tendonitis will also have some microscopic or partial tearing of the tendons. If tearing of the tendon occurs, it is usually a split along the tendon, not a breakage of the tendon into two parts. Patients with peroneal tendonitis are usually able to walk, although they may have a limp. When the tendonitis is severe, it often prevents patients from participating in dynamic sporting type activities that require sudden changes of direction.
Physical Examination: Peroneal Tendonitis
Patients will often walk with a limp. Looking at the outside of the ankle, there may be some subtle (or not so subtle) swelling behind the prominent bone on the outside of the ankle (the lateral malleolus). Pressing on this area will often create discomfort. Many patients will have a higher arched foot (subtle cavus foot), with increased ankle inversion (inward ankle motion) compared to eversion (outward ankle motion). This high arched type of foot predisposes a patient to increased loads that the peroneal tendons have to bear during walking and running. In peroneal tendonitis, the patient’s sensation and muscle strength is usually normal. However, there is a nerve (the sural nerve) that runs through the outside back part of the ankle, and this nerve may become irritated (sural neuritis) by the inflammation and swelling. This can lead to either decreased sensation or to a burning over the outside aspect of the foot (lateral side). In rare instances, some patients may have a complete tear of one of the peroneal tendons, and in this situation there may be weakness in the ability to move the foot out to the side (eversion of the foot). In patients with subluxing tendons, the tendons can be made to snap in and out of their grove.
Imaging Studies: Peroneal Tendonitis
Plain weight-bearing x-rays of the foot usually show normal joints with no evidence of arthritis. If the foot is high arched, this will likely be noticeable on the x-rays.
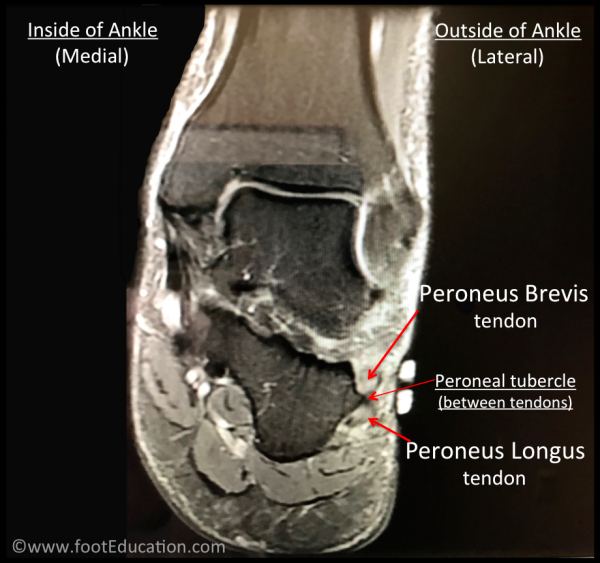
An MRI is usually not required unless surgery is being contemplated. An MRI can determine if there is tearing of the peroneal tendons (Figure 2), and if there is tearing, to determine the extent of the tear. It is also common to see abnormal fluid and edema, representing the tendonitis in the peroneal tendons (Figure 3). However, in patients 40 years of age and older partial tearing of the peroneal tendons on MRI is common! –even in patients without any symptoms! Increased fluid around the tendons is also commonly observed. On both plain x-ray and particularly on MRI, it may be possible to identify the peroneal tubercle. This is a prominence of bone on the outside of the ankle (Figure 3), which is occasionally noticeably protruding. At times the peroneal tubercle can serve as an irritant as the two peroneal tendons run on either side of this bony structure.
Patients may be frightened by the comments on an MRI imaging reports. Words such as “tear” and “degeneration” may lead the patient to be fearful of using the ankle normally in order to “protect the tendon”. However, there is good evidence to show that normal activity loads are often well tolerated despite these findings.

Treatment: Peroneal Tendonitis
Non-Operative Treatment
Most patients with peroneal tendonitis recover with non-operative treatment, even if a tear is present. Conservative treatment consists of carefully remaining active while gradually mobilizing, strengthening, and reloading the tendon as it begins to feel better. It often takes 3 or more months to feel better. Successful non-operative treatment includes:
- Ankle bracing or taping, such as the use of an ankle lacer or Kinesio Tape can be used to support the ankle and control the motion of the tendons.
- Activity Modification: A short period of limited activity over a few days or a week to allow the inflammatory response to settle may be helpful. However, in general, activity modification should include reducing activities, but not stopping completely. The tendon requires some loading to adapt, so complete rest for a prolonged period is not beneficial. It is important to pay attention to pain during activities, usually pain will decrease by performing a movement more slowly or carefully.
- Physical therapy can be helpful to select the best strengthening exercises; passive therapies are helpful in the short term, but not as effective as strengthening in the long term. Tendon massage may aggravate irritation.
- Avoid Precipitating Activities. Certain activities will exacerbate peroneal tendonitis. These can include activities with sudden cutting or changing direction motions, or anything that will increase the force through the tendons. If these can be avoided, often the tendonitis symptoms will settle.
- An Orthotic with a recessed area under the first metatarsal head: If a patient has a subtle or a not so subtle cavus (high arched) foot pattern, an orthotic with a recessed area under the first metatarsal head will often be beneficial. In patients with a high arched foot pattern, this type of orthotic can often partially or completely correct the hindfoot alignment, provided the hindfoot joints are still mobile. It would seem intuitive that patients with a high arched foot should have a high arch built into the inside of their orthotic, but in fact this is not recommended as it will have a tendency to tip the foot more to the outside, often exacerbating the load on the outside structures, such as the peroneal tendons.
- Ice applied to the area in 10- to 20-minute intervals can also be helpful in allowing some of the more acute symptoms to settle.
- Anti-inflammatory medication to decrease inflammatory response from the tendons.
Operative Treatment
In patients with a large peroneal tendon tear or a bony prominence that is serving as a physical irritant to the tendon, surgery may be beneficial. Physical irritants can include a prominent peroneal tubercle or a bone spur off of the back (posterior aspect) of the fibula (prominent bone on the outside of the ankle).
Surgery is performed to: clean up the tendons themselves (debridement or synovectomy); repair any significant tearing of the tendons; and if necessary smooth out the tract that the peroneal tendons run in. If there is tearing of the tendon, the tendon is inspected and part of the torn tendon might be removed if less than 50% of the tendon is torn. If more than 50% is abnormal, the tendon is debrided (cleaned up) and the involved tendon is sutured (transferred) to the other tendon.
Additional Surgical Procedures
Many patients may require other procedures in addition to the surgery on the peroneal tendons themselves. Additonal surgery may be performed in order to address other related problems or alter the force that the peroneal tendons are subject to. Surgical procedures may include:
- Repair of the Peroneal Retinaculum: In some individuals, the peroneal tendon problems will stem from the tendons partially (or completely) popping out of the groove (subluxing) that they normally run in, behind the fibula. This results from a tearing or stretching out of the superior peroneal retinaculum, which is a thick fibrous tissue that normally restrains the tendons. When this occurs, surgery to stabilize or repair the peroneal retinaculum may be necessary.
- Ankle arthroscopy: Patients with peroneal tendonitis may also have problems within the ankle joint itself. In this situation, an ankle arthroscopy may be indicated to examine the inside fo the ankle joint.
- Peroneal tubercle resection: The peroneal tubercle is a prominent bump of bone on the outside of the heel bone. It serves to separate the two peroneal tendons (peroneus longus and peroneus brevis) as they run along the outside of the foot (Figure 3). This bump can become enlarged due to the irritation of the peroneal tendons, and in some patients it will reach a size where it may need to be removed.
- Ankle Ligament Stabilization (ex. Brostrum procedure): Many patients with significant peroneal tendonitis requiring surgery may also have ankle instability and may require a lateral ankle ligament stabilization, such as a Brostrum procedure, in addition to the procedures on the peroneal tendons.
- Lateralizing Calcaneal Osteotomy: In some individuals with significant foot alignment issues, it may be necessary to fundamentally change the shape of the hindfoot. This is typically done with a lateralizing calcaneal osteotomy. This allows the heel to be shifted, and the distribution of force to be more even over the hind part of the foot.
- Peroneal tendon transfer and reconstruction: At times, one of the peroneal tendons (usually the peroneus brevis) may have a tear or degeneration that is severe and prevents repair. In this situation, the torn portion of the tendon is removed and the remaining part of the tendon is stitched on to the side of the intact tendon. If both tendons are damaged beyond repair, then if there is a functioning muscle after removing the damaged tendons, the gap in the tendon is reconstructed with a tendon taken from a donor (allograft tendon), or replaced with another tendon from the vicinity.
Potential Surgical Complications
Potential complications of surgery can occur. These include:
- Deep wound infection.
- Wound healing problems
- Sural Neuritis. The sural nerve, which innervates the outside of the foot, is often stretched or injured in the surgical approach and can become scarred or injured in the course of the surgery.
- Deep Vein Thrombosis (DVT)
- Pulmonary Embolism
Edited on May 27th 2025
Previously Edited by Gwyneth deVries, MD, and Vinod Panchbhavi, MD