Bunions
(Hallux Valgus)
Edited by Eric Malicky, MD
Summary: Bunions
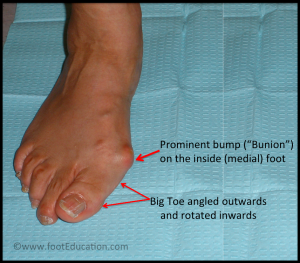
A bunion (aka: Hallux Valgus) is a common foot condition associated with a prominent bump on the inside of the forefoot (see Figure 1). The word bunion originates from the Latin root for the word “turnip.” Bunions can lead to discomfort over the bump, especially if patients wear tight fitting or stiff shoes. It is common for bunions to run in a family and gradually worsen with time. Most bunions can be treated without surgery. However, surgery is an option for the few patients who continue to hurt (despite non-surgical care).
Figure 1: Bunion Deformity
Click Here for a Summary Handout about Bunions
Read More: 5 Things you probably didn’t know about bunions!
Clinical Presentation: Bunions
Patients with bunions will often describe pain over the prominent bump on the inside of their forefoot (the medial eminence). They may also experience pain under the ball of the foot near the base of the second toe. Symptoms vary in severity and can occur with standing, walking, or even at rest. There is no direct connection between the size of the bunion and the patient’s symptoms. Bunion pain is often worse with restrictive shoe wear (either a narrow or stiff toe box).
Bunions can run in the family. A positive family history for bunions may be the single greatest risk factor for developing the condition. Often a patient will recall a first-degree relative (parent or sibling) having similar foot issues (bunion, flatfoot, toe deformity).
Bunions occur from a shift in the bones around the great toe. The big toe (the hallux) drifts toward the little toes (laterally) after its base (the first metatarsal) shifts to the midline (medially). The visible bunion reflects a combination of the movement of these bones, the resultant prominent first metatarsal bone (Figure 2), and any tissue swelling around this joint (from rubbing). In some cases, the big toe joint deformity can lead to arthritis.
Painful bunions simply result from the outer pressure of restrictive shoes on this area and the irregular joint stresses occurring from the toe deformity.
Physical Examination: Bunions
Physical examination typically reveals a prominent bump on the inside of the forefoot due to changes in the position of the first metatarsal bone and great toe. Drifting of these bones cause the big toe joint to rotate out of place (“subluxate”). This often results in redness and swelling along the bunion and can be painful to touch.
Patients may also have a thickening of the skin (callus) at the base of their second toe in the sole of the forefoot because as the first toe drifts, the ball of the foot carries more weight, and this can be an additional source of pain (metatarsalgia).
Imaging Studies: Bunions
To fully evaluate a bunion it is necessary to obtain standing x-rays of the foot. These x-rays are typically taken from the top (anteroposterior) (see Figure 2) and from the side of the foot. A physician can use these x-rays to classify the extent of the bunion deformity.
Figure 2: X-ray showing bunion

The degree of big toe angulation (Hallux Valgus Angle) can be measured on x-ray (Figure 2).
- Mild deformities are considered if the big toe angulation is <20 degrees,
- Moderate deformities from 20-40 degrees,
- Severe deformities the great toe angulation is greater than 40 degrees.
Treatment
Non-Operative Treatment: Bunions
The initial treatment for almost all bunions should be non-operative. Symptoms can often be greatly improved with simple interventions. Non-operative treatment may include adjusting the shoes or trying common products available at pharmacies, sporting goods stores, and through the internet:
- Properly fitted shoes: Properly fitting comfort shoes with a wide non-constrictive toe box (with soft materials) can be quite helpful in reducing the irritation over the prominent bunion. In some instances, it is helpful to stretch the inside aspect of the shoe. Jamming a foot with a bunion into a constrictive shoe will likely lead to the development of uncomfortable symptoms. Inspect your shoes/boots to see if the area over the bunion can be stretched. You might be surprised how easy this can be accomplished with a relatively inexpensive “shoe stretcher.”
- Bunion pads (bunion sleeve): Bunion pads may also be helpful in decreasing the symptoms associated with the bunion (Figure 3). This thin silicone material lessens the rubbing over the bunion and decreases the irritation. This should be combined with comfortable wider/soft shoes.
- A silicone toe spacer placed between the great toe and the second toe can help to straighten the bunion deformity and help re-align the big toe joint.
- Soft shoe inserts: Over-the-counter soft orthotics may also help bunion symptoms especially if there is more pain beneath the ball of the foot. Orthotics with a slight arch may be helpful for patients that have flat feet. Don’t forget that you may need to purchase a slightly larger shoe to comfortably wear the inserts.
- Bunion splints have often been used to treat the symptoms associated with hallux valgus. These splints are typically worn at night in an effort to reduce the bunion deformity. There is no evidence to suggest that these splints will slow the toe deformity but some patient’s feel some relief when wearing them.
Figure 3: Bunion Sleeve -soft material pads the prominent bunion

Operative Treatment: Bunions
Surgery should only be considered in patients who have failed non-operative options. Bunion surgery has the most success in patients with moderate to severe pain associated with the bunion, and SHOULD NOT be used solely for cosmetic reasons. Furthermore, all surgical patients must realize the prolonged time required for complete recovery from this bunion surgery.
The primary indication for operative intervention is pain that is not relieved by appropriate non-operative management. Although symptom-free bunions can slowly worsen or increase in size over time, surgical treatment is NOT recommended unless significant pain symptoms develop. “Preventative bunion surgery” is not recommended and can lead to disappointment.
The prolonged recovery time (3 – 12 months) associated with most bunion operations, combined with the potential for complications means that patients should be thoughtful about considering bunion surgery.
There are many different procedures that have been described to correct bunions. The type of operation your foot surgeon recommends to correct your bunion should be dictated by the severity of your bunion deformity and the surgeon’s preference. There are well over 150 different bunion correction procedures described in the orthopaedic literature. However, the broad categories of bunion correction procedures are listed below, some of which link to a page where the surgery and recovery are described in detail.
- “Simple” bunionectomy: Removal of the prominence on the inside of the foot (medial eminence).
- Distal metatarsal osteotomy (Chevron): with great toe soft-tissue tightening (medial capsular tightening and distal soft-tissue repair). This involves cutting the bone near the toe joint.
- Proximal metatarsal osteotomy (Ludloff, Cresentic, SCARF, medial opening wedge): with great toe soft-tissue tightening (medial capsular tightening and distal soft-tissue repair). This also involves cutting the metatarsal bone along it’s shaft.
- Lapidus hallux valgus correction: This involves re-alignment and fusion of the first tarsometatarsal joint with distal soft tissue procedure.
- Great Toe Fusion (1st MTP joint arthrodesis): usually reserved with associated toe arthritis
- Akin osteotomy: Realignment bone cut at the base of the big toe
- Removal of the medial eminence with suture stabilization of the first and second metatarsals
- Keller joint arthroplasty: Removal of the base of the great toe joint bone.
Please remember, bunion surgery is a serious operation and should not be considered “simple” regardless of your perception. There can be many misleading commercials suggesting an easy and quick recovery from bunions surgery but please be mindful of the risks. Afterall, your feet matter and shouldn’t be taken for granted.
When to see an orthopaedic foot specialist
For most people, sufficient education combined with following the above non-operative treatment measures will result in good function with fewer symptoms. Reasons to seek consultation with an orthopaedic foot specialist include:
- Persistent bunion pain that does not improve with shoe modification and other non-operative measures.
- Worsening bunion deformities that begin to involve the second toe, altering its alignment or causing additional pain.
Click Here for a Summary Handout about Bunions
Read More: 5 Things you probably didn’t know about bunions!
Edited June 6, 2020
Previously edited by Daniel Guss, MD, M.B.A. and Jean Brilhault, MD
mf/ 7.24.18
